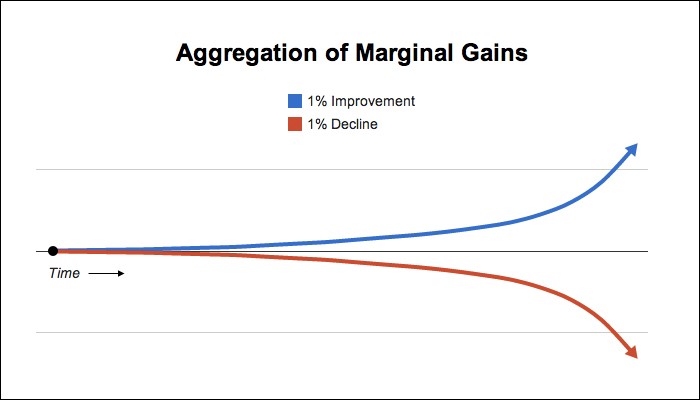
Efficiencies in scheduling can be crucial to positively impacting revenue at your ambulatory surgery center. Maximizing scheduling efficiency creates room for more procedures. Even if you gain only one or two procedures each day, these marginal gains can easily increase your bottom line. Therefore, taking steps to cultivate efficiency is an essential strategic initiative.
Here are seven ways to create efficiency in your ASC’s scheduling process.
1. Encourage your physicians’ offices to schedule cases as far in advance as possible. Cases scheduled well in advance of surgery dates allow surgery center personnel adequate time to prepare for patients. Obtaining pre-authorizations from some insurance companies can take several days to complete. Surgery center staff must call patients in advance of their procedure to review their medical history and discuss financial obligations. Managers staff the center based on the number and types of cases on the schedule. At times, center personnel need to pre-order special equipment, medical supplies, or patient-specific implants. If your physicians’ offices encounter changes in their surgeons’ schedules – cancellations, add-ons, time changes, or order changes, for example – encourage them to communicate those changes to you as quickly as possible. Discuss ahead of time the preferred form of communication for your center – phone, email, fax – to create efficiencies for their team and yours.
2. Establish a strong working relationship with your physicians’ offices to obtain accurate information. Coordinating patient care requires teamwork. When your ASC serves as an extension of each physician’s practice, the care continuum is virtually seamless. It is crucial to obtain scheduling forms from your physicians’ offices with comprehensive patient information and up-to-date copies of both sides of the patients’ insurance cards. This information assists in determining if patients are viable candidates for surgery at your facility from both a clinical and third-party payor coverage standpoint. If the surgery or procedure falls under workers’ compensation, ask your physicians’ offices to include adjustors’ names and phone numbers.
3. Schedule patients with special needs and your more extensive/high acuity cases at the beginning of the day. Include small children and patients with chronic illnesses, such as diabetes and sleep apnea, in this classification. Scheduling these cases first allows lengthier recovery times to be more easily accommodated. Additionally, caring for these patients during usual working hours prevents staff from having to stay late or accumulate costly overtime hours.
4. Schedule specialties in the same room whenever possible. This prevents staff from spending valuable time moving equipment from room to room, leading to shorter turnover times.
5. Schedule similar surgical sites consecutively (i.e., right vs. left, shoulder vs. knee). As an example, for orthopaedic arthroscopy cases, you may prefer to keep all the shoulder cases in line and then move to knee arthroscopies. This will reduce the need to change positioning devices and room set up between cases. Speeding up room turnover, anesthesia set up, and the overall flow of surgery, typically yields happier surgeons!
6. Know what you have to work with. Larger facilities may have the ability to set up rooms by specialty. Smaller facilities will need to focus on how to best move and position equipment. Train your staff to think strategically about these types of things based on your center’s unique characteristics.
7. Communicate your ASC’s patient criteria to your surgeons and their staff. Patient safety is a priority. When your physicians and their office staff understand the contraindications and anesthesia requirements at your center, they can schedule their patients at the appropriate facility.
After you determine the best efficiency workflow processes for booking procedures at your facility, educate physicians, their scheduling staff, and your facility personnel on how they work and why they are set up that way. Scheduling efficiencies go a long way toward creating higher satisfaction for your team and physicians. More importantly, scheduling efficiencies create opportunities to add more cases and increase your ASC’s revenue.
Kelli McMahan – VP of Operations